How Meghalaya state’s integrated approach is leading the way to Universal Health Coverage in India
Each year, 55 million Indians are pushed into poverty due to high out-of-pocket expenditure on health, with over 17% of households incurring catastrophic levels of expenses every year. The High-Level Expert Group envisioned Universal Health Coverage (UHC) for India by 2022, however the country is yet to ensure healthcare for all.
Equity is the guiding principle to achieve Universal Health Coverage in this diverse country where geography and socio-economic status varies remarkably for a population needing local solutions. In India, health is a state matter when it comes to driving policies and implementation, which means the state can custom design solutions in accordance with the needs of the population.
Have you read?
- Mainstreaming universal health, with Japan at the helm as a long-lived nation
- Will universal health coverage deliver health for all by 2030?
- Governments urged to invest in healthcare systems despite global economic uncertainty
Meghalaya state, in northeastern India, is leading the way to ensure UHC through its State Health Enhancement Project (SCEP). As a mountainous state with the largest number of remote inhabitants in the country, geographical challenges are foremost in delivering healthcare to its citizens.
Through the Program Driven Iterative Adaption approach, the state deep-dived into the challenges which revealed that short birth spacing leads to high maternal mortality, anaemia, teenage pregnancy, remoteness, poverty and low trust in health systems. This led the state to draft and release the state health policy in 2021 outlining its commitment to assuring Universal Health Coverage for its population.
SCEP is a 3D model which aims to change the inverted pyramid model of healthcare in India, which focuses on tertiary healthcare and a quantum of primary care, to a more robust model of preventive healthcare and wellbeing.
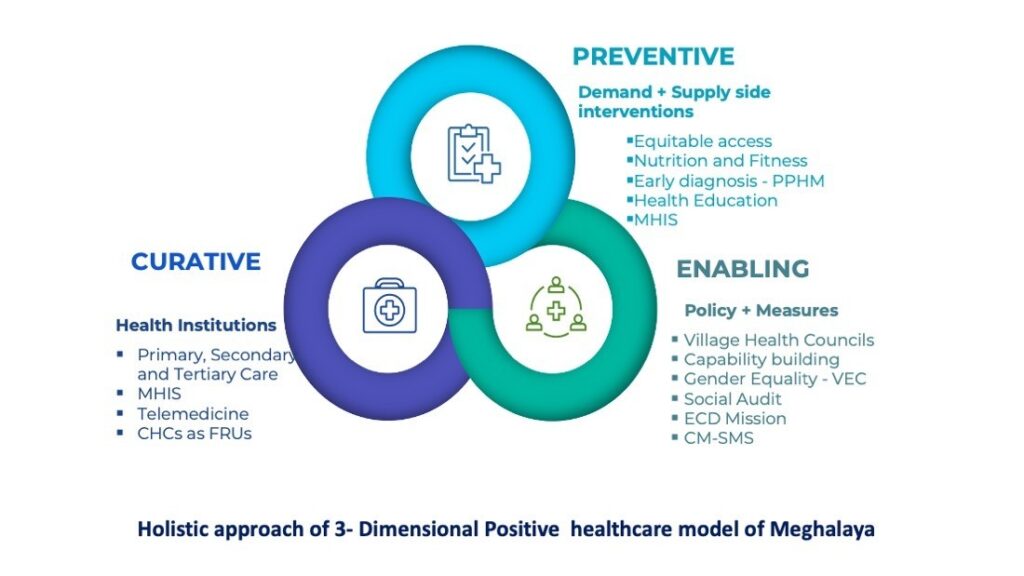
The Universal Health Coverage takes into account both demand and supply side interventions, with emphasis on Comprehensive Primary Health Care.Image: Source: Health and Family Welfare Department, Meghalaya.
Preventive health component
Universal Health Coverage takes into account both demand and supply side interventions, with emphasis on Comprehensive Primary Health Care (CPHC) envisioning reaching the entire population for annual screening of common ailments and health needs. Under the Smart Village Movement Project, the government is working with UC Berkeley to leverage digital technology and AI to identify health trends and design future interventions.
Curative component
This is being addressed through the state specific Megha Health Insurance Scheme which covers everyone in the state irrespective of their socio economic and caste status and also makes Meghalaya the first state in the country to provide out-patient department (OPD) coverage of INR 30,000 – over and above the coverage under Pradhan Mantri Jan Arogya Yojna (PM-JAY).
In addition, the state has launched the Chief Minister’s Safe Motherhood Scheme to address critical gender and poverty issues to ensure safe labour and delivery. The spouses of high-risk pregnant mothers are given wage compensation to ensure they are brought to their nearest healthcare institutions. This intervention is also designed to leverage the trust of traditional birth attendants who can play a key role in reducing the high rate of MMR in remote villages.
Mothers App has been developed to record the data of all expectant mothers and predict high-risk pregnancies, allowing healthcare professionals to bring them to health facilities before an emergency arises.
Meghalaya has also collaborated with Tamil Nadu, the southern Indian state which has stronger public health systems, to train its current workforce for specialist treatment and fill up vacancies at First Referral Units (FRUs).
Enabling component
Driven by policy and measures, the state has come up with the unique concept of Village Health Councils (VHCs), which are elected local health bodies to inculcate a sense of community participation. Gender equality has been at the heart of this approach by having representations of women in rural bodies.
VHCs solve the demand side problem of healthcare as they hold the state systems accountable for delivery of services by highlighting gaps and needs. The women’s Self Help Groups (SHGs) are an integral part of VHCs – discussing common health challenges and implementing health infrastructure projects based on the needs of the community.
Social audit law also gives power to the people to audit 21 welfare programmes in the state. Early Childhood Development (ECD) has been launched to unleash the full potential of children by leveraging the advances made in the science of early childhood. The Anganwadi Centres (AWC) are being transformed into ECD centres where children and breastfeeding mothers are provided with eggs and cooked meals.
Children will spend one-fourth of their time at AWC, which will also provide a stimulating environment through learning activities – helping to build the future human capital of the state with enhanced cognitive and socio-emotional capabilities. Additional care-givers and early childhood educators are being provided at AWCs – leveraging the existing social capital of active women SHGs nurtured in every village under the National Rural Livelihoods Mission. In addition, parents are regularly supervised through house visits.

What is the impact of Universal Health Coverage?
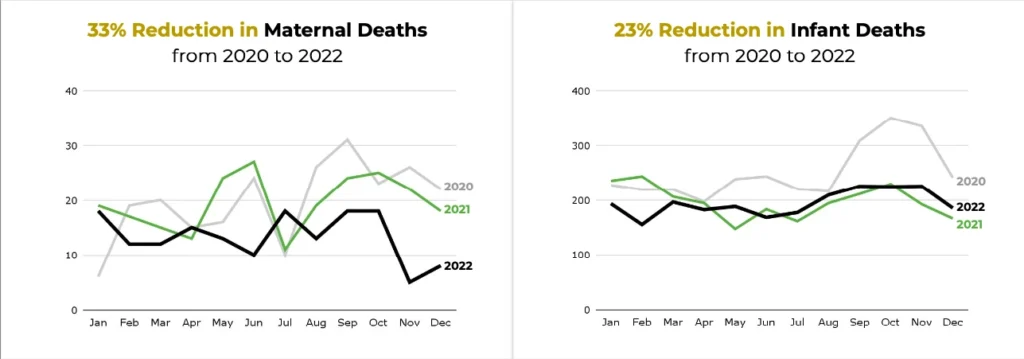
The 3D model of SCEP relies on local solutions to local problems and has shown great results within a year of its implementation. There has been a 23% reduction in infant deaths and a 33% reduction in maternal deaths from 2020 to 2022, which has instilled a strong sense of purpose in the health workforce.
What are the key findings?
The World Health Organization (WHO) recommends reorienting health systems to primary healthcare (PHC) which enables universal, integrated access in everyday environments to the full range of quality services and products people need for health and wellbeing, thereby improving coverage and financial protection. The majority of essential Universal Health Coverage interventions (90%) can be delivered through PHC and there are significant cost efficiencies in using an integrative PHC approach.
The long-term success of India’s reform towards Universal Health Coverage depends on how it is connected to a well-functioning and adequately staffed primary healthcare system, one that goes beyond curative care to encompass broader health promotion and prevention efforts which are necessary to improve population health. Meghalaya has shown the way forward by following a holistic approach of preventive, curative and enabling healthcare.
Source: weforum.org